What is normal infant jaundice?
Jaundice, yellowing of the skin, eyes, gums and inner lips, is common and normal in breastfeeding infants. The yellow colour is caused by extra bilirubin in the baby’s blood. Bilirubin is produced when red blood cells break down. In the womb, your baby has extra red blood cells to bring oxygen from the placenta. Once your baby is born, he uses his lungs to get oxygen. These extra blood cells are no longer needed. They break down to be recycled in your baby’s body. One byproduct is a yellow pigment called bilirubin. It is removed naturally from your baby’s body in the stools (poops). The first stool, meconium, has a large amount of bilirubin. This is why it is black in colour. The more your baby feeds in the early days, the quicker the bilirubin leaves your baby’s body. Most of the bilirubin (98%) will be eliminated in your baby’s early stools. Babies with darker skin tones may not show the yellowing effect of jaundice, so they should be observed carefully.
Normal, mild jaundice generally takes a few days to appear. The level rises slowly, usually peaking between days 3 and 5 at less than 12 mg/dl. (Between days 3 and 5 is also when your milk production should increase dramatically. When your baby is feeding well, this results in more frequent and larger poops.) Mild jaundice usually resolves without treatment other than frequent and effective feeding. Adequate milk intake is what helps your baby clear the bilirubin from his body. Some babies will have mildly elevated bilirubin levels for as long as 15 weeks or longer.
What is suboptimal intake jaundice?
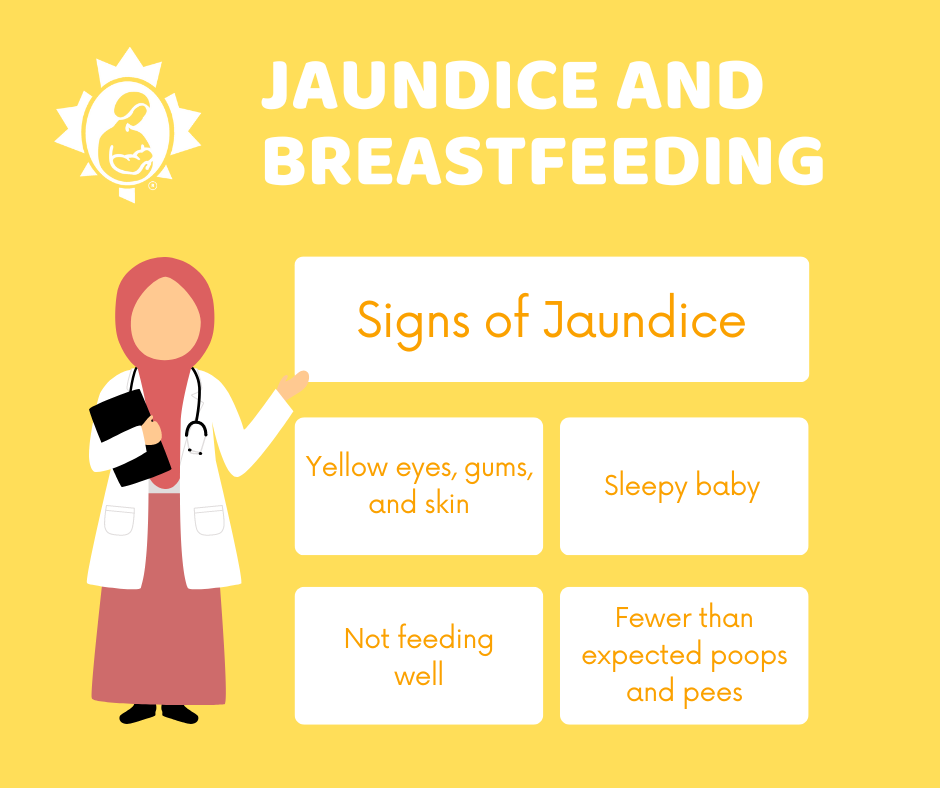
Suboptimal intake jaundice occurs when a baby is not getting enough colostrum/milk to eliminate the bilirubin. When there is not enough milk intake, bilirubin is not eliminated as quickly as it should be. If the bilirubin is not eliminated quickly, it is absorbed from your baby’s gut back into the blood at higher levels. This causes more yellowing of your baby’s skin and eyes. This increase in yellowing may not be recognized in a baby with darker skin colour. It’s helpful to check the gums and inner lips. Your baby may become more and more sleepy, making feeding even more challenging. Your baby’s bilirubin levels will be monitored by your healthcare provider. It is essential that your baby gets more to eat. Phototherapy treatment is often required to help settle things down.
Is jaundice dangerous?
Sometimes it is. But mild to moderate jaundice is not dangerous. Bilirubin is a powerful antioxidant and can play an important and beneficial role in protecting newborn health.
However, if bilirubin reaches too high a level, it can cause injury to a baby’s brain. Safe bilirubin levels are determined individually based on gestational age, weight and your baby’s overall health. Small or premature babies are at risk of brain injury from a lower level of bilirubin than can be tolerated by a full-term baby.
Jaundice that appears within the first 24 hours, rises quickly, and reaches higher than 17 mg/dl in a full term baby is indicative of a more serious problem. This is sometimes called pathological jaundice. This is often caused by other factors, not a lack of milk. It needs to be assessed and treated promptly without interrupting breastfeeding.
Risk factors for jaundice in newborns
- Delayed milk production. There are many reasons why breastfeeding might get off to a slow start. Cesarean section birth and first time pregnancy are two common situations where it helps to take extra care with getting breastfeeding established.
- Premature birth.
- Birth earlier than 38 weeks.
- Small for the baby’s gestational age.
- Bruises in the baby’s head from the birth.
- Maternal diabetes.
- Rh sensitization.
- Family history of jaundiced infants.
Boys are more likely to be jaundiced than girls. Asian babies are most likely to be jaundiced, followed by Indigenous North American babies, Caucasian babies and finally African American babies. O blood type and RH negative mothers are also more likely to have jaundiced babies.
Preventing high jaundice levels
- Breastfeed early and frequently. Start as soon after birth as possible. A good latch is important for effective milk removal. See Positioning and Latching. Early feedings help your baby pass the meconium or first stool quickly.
- Lie-back in a comfortable, reclined position that supports your back. Hold your baby skin to skin and chest to chest. The laid-back position allows your baby to use her inborn reflexes to find the breast and latch. It also frees your hands so you can help, as needed. You and your baby can feed like this for many days. It will help you get to know each other and learn how to get a good latch. Continue putting your baby to breast frequently in the early days. Respond to all feeding cues.
- Avoid giving your baby water or glucose. This will not prevent jaundice or bring down bilirubin levels. It will interfere with your baby getting enough milk.
- Arrange a visit with your baby’s healthcare provider within two days of discharge from a hospital birth.
- Consult your baby’s healthcare provider if your baby is:
~sleepy.
~not feeding well.
~not pooping as expected.
Sleepiness and poor feeding are signs of high jaundice levels.
Treatment for jaundice
Bilirubin levels are checked by a blood test. Your baby’s healthcare provider may order a blood test if:
- your baby is sleepy and not feeding well.
- much of your baby’s body looks yellow.
- your baby’s skin and eyes started turning yellow within the first 24 hours.
Treatment of severe jaundice may require your baby to spend time under phototherapy lights. These special lights help break down the bilirubin so it can be removed in your baby’s urine as well as the stool. Your baby’s eyes are covered while under these lights. Separation during this treatment can be upsetting. You can stay with your baby, and in most cases, take your baby out from under the lights to feed. Placing your baby skin to skin during these feedings encourages instinctive feeding behaviours. Holding your baby skin to skin also calms you.
Your baby may also require supplementation with expressed milk, donor milk or formula. This may be necessary if your baby is sleepy and not feeding well. It may also be necessary if your milk production is slow to increase. Your baby needs food to eliminate the bilirubin. If your baby is not getting enough milk at breast, supplementation is needed to remove the bilirubin from your baby’s body. You could supplement with a cup, spoon, at-breast supplementer or bottle. See How to Protect Breastfeeding while Supplementing.
Treatment of high bilirubin levels usually takes a few days. It is important to express your milk during this time so that you can provide your own milk for your baby and establish a plentiful milk supply. See Establishing Your Milk Supply and Breast Pump vs Hand Expression. Once your baby’s bilirubin levels are dropping, your baby will be more alert and will feed better.
What is prolonged (late-onset) jaundice?
Sometimes jaundice lasts beyond the first two weeks of life. This is often called prolonged, late-onset, or breast milk jaundice. Bilirubin can sometimes remain in your baby’s body at moderate levels for many weeks. This is more common in babies who had higher bilirubin levels earlier. Babies with late-onset jaundice are alert, feeding well, gaining weight and growing. As long as bilirubin levels stay below about 20 mg/dL, prolonged jaundice resolves without any treatment by about 12 to 15 weeks. Some healthcare professionals may recommend temporary weaning, but this is not beneficial or necessary. (For information to share with your healthcare provider, see Academy of Breastfeeding Medicine Protocol #22 Jaundice).
If you have any breastfeeding questions or concerns, contact your local La Leche League Canada Leader who can provide you with support and information.
If you have found this helpful, please consider making a donation to LLLC.
References
Flaherman, V.J., Maisels, M.J. and the Academy of Breastfeeding Medicine. (2017). ABM Clinical Protocol #22: Guidelines for Management of Jaundice in the Breastfeeding Infant 35 Weeks or More of Gestation—Revised 2017, Volume 12, Number 5, 2017. DOI: 10.1089/bfm.2017.29042.vjf
Mohrbacher, Nancy. (2020). Breastfeeding Answers: A Guide for Helping Families, Second Edition. Nancy Mohrbacher Solutions, Inc., 245-246.
Updated 2022
